Key Takeaways
- Clinical-Grade Accuracy & Compliance: Medical terminology recognition, HIPAA-compliant architecture, encryption, PII redaction, and a signed BAA must be non‑negotiable.
- Workflow Integration: The platform should plug into your EHR/EMR, telephony, contact center, and CRM systems so transcripts, notes, and tasks flow automatically into existing workflows.
- QA & Compliance Automation: Look for 100% interaction coverage, automated scoring against healthcare-specific scorecards, real-time compliance alerts, and coaching insights, not just call recordings.
- Patient Experience & ROI Impact: The solution should help boost call-to-appointment conversions, reduce no-shows and complaints, and cut QA/admin time so clinicians spend more time on patient care.
- Scalability & Change Management: Ensure it can handle your current and future volume, support multi-site operations, and include training, pilots, and adoption support so staff see it as a burden reducer, not a surveillance tool.
A. What is conversation intelligence in healthcare?
Conversation intelligence uses AI to analyze patient-staff interactions across phone calls, video consultations, and chat channels.
It’s not basic call recording or transcription. Those tools capture conversations but don’t analyze them. Conversation intelligence goes several steps further:
- Transcribes conversations with medical terminology accuracy
- Analyzes sentiment, compliance adherence, and communication patterns
- Scores interactions against your quality frameworks automatically
- Alerts supervisors to compliance violations in real-time
- Identifies coaching opportunities based on actual conversation data
Healthcare organizations need it now because regulatory scrutiny is intensifying. In 2025, HIPAA violations cost between $145 to $2,190,294 per violation. Manual monitoring can’t scale to catch every risk. Staff burnout is at record highs, with nurses spending hours on administrative tasks instead of patient care.
According to a 2025 healthcare workforce study by the American Hospital Association, administrative burdens consume resources that should support direct care. Conversation intelligence automates documentation, reduces paperwork, and frees clinical staff to focus on what matters most.
B. The healthcare communication gap: where conversation intelligence fits
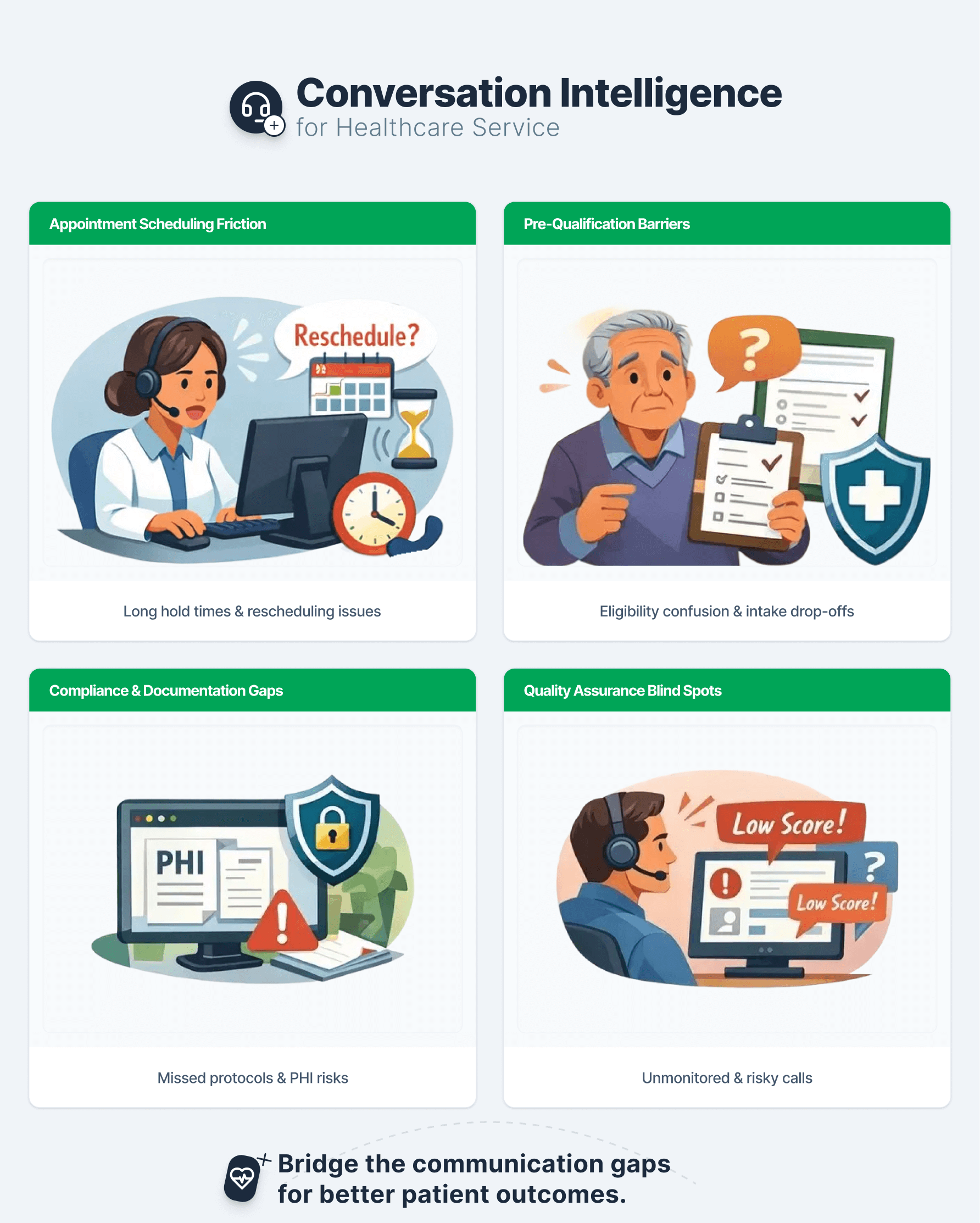
Healthcare providers face four critical communication challenges that directly impact patient outcomes and revenue. Have a look at the real communication gaps that cost you patients, revenue, and compliance.
1. Appointment scheduling friction
Scheduling friction shows up as long handle times, abandoned calls, and repeated rescheduling requests. Conversation intelligence reveals which scripts, queues, and time slots correlate with these outcomes.
In many rollouts, teams discover that simple tweaks like confirming insurance earlier or offering clear telehealth instructions cut repeat calls and shorten queues.
2. Pre‑qualification barriers
Pre‑qualification barriers emerge when patients struggle with eligibility questions, coverage details, or pre‑visit instructions. Conversation intelligence captures hesitations, repeated questions, and negative sentiment around specific parts of the script.
With that data, you simplify language, re‑order questions, or give agents better on‑screen guidance. Over time, you see more completed intakes and fewer frustrated callers abandoning the process.
3. Compliance and documentation gaps
Compliance and documentation gaps are often invisible with manual QA. Only 1-2% of calls usually get reviewed in detail, even in regulated settings. That leaves you exposed to PHI handling, identity verification, disclosures, and consent.
Conversation intelligence monitors 100% of interactions, automatically redacts PHI/PII, and flags calls where agents miss required language or deviate from policy. Compliance teams then use a searchable trail instead of random samples and frontline memory.
4. Quality assurance blind spots
Quality assurance blind spots appear when supervisors rely on random call picks and subjective scoring. Teams know there are issues, but cannot say how often they occur or where.
With platforms like Enthu’s QA Agent, every interaction gets scored, and low‑scoring or high‑risk calls surface automatically in dashboards. Supervisors then spend time on coaching, calibration, and process fixes instead of hunting for examples.
C. Key benefits of conversation intelligence for healthcare services
Conversation intelligence delivers benefits in many areas. Here are the top practical wins you can expect from conversation intelligence, from better patient experiences to tighter compliance.
1. Improve patient engagement & retention
Patient engagement starts with the first phone call.
Conversation intelligence identifies exactly where patients disengage during scheduling. You’ll see which questions confuse callers, which staff members convert appointments most effectively, and where processes break down.
You can optimize pre-qualification processes by tracking which information collection methods work best. Staff who explain “why we need this information” before requesting details get 40% better completion rates than those who jump straight into questions.
Engagement improvements directly reduce patient churn. When patients feel heard, understood, and efficiently served, they return for ongoing care and refer others.
2. Ensure HIPAA compliance & risk mitigation
You ensure HIPAA compliance by treating conversation intelligence as part of your regulated data environment from day one.
Conversation intelligence provides four critical compliance capabilities:
- PII detection and masking automatically identify protected health information in transcripts. The system redacts patient names, social security numbers, and medical details from searchable records. You maintain audit trails without exposing sensitive data unnecessarily.
- Consent management tracking verifies that staff obtained proper authorization before discussing medical information. The AI flags interactions where consent verification was skipped or incomplete. Supervisors receive immediate alerts to address gaps before they become violations.
- Audit trail automation creates bulletproof documentation for regulatory audits. Every conversation gets logged with full metadata: participant identity verification, topics discussed, consent obtained, and information disclosed. When auditors request evidence, you provide complete records instantly.
- Regulatory reporting becomes automatic instead of manual. The system generates compliance scorecards showing adherence rates across teams, locations, and interaction types. You identify compliance trends before they escalate into violations.
3. Automate quality assurance at scale
You can’t listen to every call. Your QA team reviews a tiny sample, usually 2-5% of interactions. That means quality issues, compliance gaps, and coaching opportunities remain hidden in the 95% of unmonitored conversations.
Conversation intelligence analyzes 100% of interactions automatically. Here’s what changes:
- Automated scoring against compliance frameworks evaluates every conversation against your quality criteria. Did the agent verify patient identity? Obtain consent? Provide accurate information? Demonstrate empathy? The system scores all factors consistently, eliminating human bias and coverage gaps.
- Real-time alerts for compliance violations notify supervisors immediately when issues occur. If staff discuss protected health information without verification, supervisors receive alerts within seconds. They can intervene, correct the interaction, and coach the employee before more violations happen.
- Coaching recommendations based on QA findings target specific improvement areas. Instead of generic training, managers see exactly which conversations demonstrate gaps. They share actual examples with staff: “Here’s where you forgot consent verification. Here’s how your peer handled the same situation correctly.”
4. Measure ROI & operational efficiency
Executives need proof that conversation intelligence delivers value.
These four metrics demonstrate clear ROI:
- Call-to-appointment conversion rates show scheduling efficiency improvements. Track how many patient calls result in booked appointments before and after implementing conversation intelligence. A typical improvement ranges from 15-30% as you identify and fix conversion barriers.
- Cost per patient acquisition decreases when you optimize intake processes. Calculate total contact center costs divided by new patients acquired. Organizations typically see 20-35% reduction in acquisition costs by improving scheduling efficiency and reducing no-shows.
- Staff productivity metrics quantify administrative time savings. Automated documentation reduces nurse paperwork by 30-45 minutes per shift. Calculate hourly wages times saved hours times number of staff.
- Compliance incident reduction prevents costly violations. Track HIPAA incidents, patient complaints, and regulatory findings before and after implementation. One violation costs $100 to $2 million. Preventing even one serious incident pays for years of conversation intelligence investment.
D. Real-world use cases: conversation intelligence in healthcare
Now you move from theory to practice with concrete healthcare use cases. You see how organizations like yours apply conversation intelligence to improve chronic disease management, streamline patient engagement, and reduce post-acute care costs.
Use case 1: Mount Sinai Medical Center scales chronic disease management
The challenge they faced
Mount Sinai Medical Center, Florida’s largest private teaching hospital, needed to monitor thousands of chronic disease patients across 13 locations. Manual check-ins couldn’t scale, leaving patients disconnected between clinic visits and at risk for complications.
The solution they implemented
They partnered with HealthSnap to launch AI-powered Remote Patient Monitoring and Chronic Care Management. The platform automates patient conversations, collects health data through natural dialogue, and integrates directly with EPIC. AI flags concerning patterns while care teams focus on patients needing intervention.
The results they achieved
Within months, Mount Sinai reached 4,000 active patients managing hypertension, diabetes, CHF, and COPD, with plans to serve 10,000 patients. The HITRUST-certified platform enabled proactive care at scale without overwhelming staff, transforming chronic condition management across their entire primary care population.
Use Case 2: Northwell Health cuts post-acute care costs
What was happening
Northwell Health patients felt disconnected during critical recovery periods after discharge. This communication gap led to avoidable complications, unnecessary readmissions, and rising post-acute care expenses across multiple hospitals.
How they fixed it
They launched Northwell Health Chats powered by Conversa’s AI platform. Patients receive SMS notifications requiring no app download. The AI personalizes conversations based on individual conditions, checks in every one to four days, and routes responses to care navigators who identify which patients need immediate attention.
What changed
Serving several thousand patients across oncology and surgical populations, they achieved 97% patient satisfaction and measurable cost reductions. One-third of conversations are patient-initiated, giving patients on-demand access without requiring 24/7 staff availability. Recovery monitoring became continuous instead of sporadic.
Use Case 3: Helvetia transforms insurance claims processing
The Original Problem
Swiss insurer Helvetia processed bicycle theft claims through multiple manual steps, authentication, information collection, verification, and payment processing. Each claim required days of back-and-forth communication, creating delays and frustration while consuming massive staff resources.
The AI-powered approach
They deployed conversational AI on Facebook Messenger to handle claims end-to-end. The assistant authenticates users through dialogue, collects necessary details naturally, verifies information instantly, and triggers automated payment through robotic process automation—all without human intervention for routine cases.
The business impact
Processing time dropped from days to minutes through instant verification. Integrated fraud detection flags anomalies before approval, catching issues manual review might miss. Operational costs decreased significantly as staff shifted from routine data collection to complex cases requiring judgment. For healthcare, this model applies directly to insurance verification, prior authorization, and benefits explanation, administrative conversations that consume enormous resources.
E. What implementation challenges will you face with conversation intelligence (and how do you solve them)?
You will face four predictable challenges: data privacy, integrations, change management, and metric design. Addressing them early makes your rollout smoother.
Challenge 1: Data privacy & HIPAA integration
Your conversation intelligence platform must sign a Business Associate Agreement (BAA). Without a BAA, sharing PHI with the vendor violates HIPAA regardless of technical safeguards in place.
The solution: It includes end-to-end encryption for all recordings and transcripts. Storage must meet HITRUST CSF certification standards. PII detection and automatic redaction protect sensitive information in searchable records. Verify your vendor provides dedicated healthcare infrastructure, not generic business communication tools adapted for healthcare use.
Challenge 2: integration with existing EHR/call systems
Most healthcare organizations use EHR/EMR systems, scheduling platforms, contact center software, and CRM tools. Your conversation intelligence solution needs pre-built integrations or robust APIs to connect these systems.
The solution: Look for platforms offering structured task execution where each operation (ID verification, scheduling, documentation) connects to specific tools. This separation improves safety and oversight compared to monolithic systems.
Challenge 3: Change management & staff adoption
Position conversation intelligence as reducing administrative burden, not monitoring staff. Emphasize how automated documentation gives nurses 30-45 minutes back per shift for patient care instead of paperwork.
The solution: Start with a pilot program in one department. Demonstrate quick wins like reduced documentation time or caught compliance gaps. Let staff experience benefits firsthand before rolling out organization-wide.
Challenge 4: Defining quality metrics for the healthcare context
Generic contact center metrics don’t translate directly to healthcare. Average handle time matters differently when complex medical questions require thorough explanations. Talk-to-listen ratios need adjustment for patient-centered communication styles.
The solution: Build healthcare-specific quality scorecards that balance efficiency with thoroughness. Include metrics like:
- Consent verification completion rate
- Patient identity authentication compliance
- Empathy indicators during difficult conversations
- Clinical information accuracy
- Follow-up scheduling completion
- Patient education quality
Weight metrics according to your organization’s priorities and regulatory requirements.
F. Conversation Intelligence vs. Traditional QA Methods
Conversation intelligence differs from traditional QA because it scores every interaction and focuses human effort where it matters most. Manual methods can never reach that scale.
| Factor | Manual QA | Automated Conversation Intelligence |
| Coverage | 2-5% of interactions sampled | 100% of interactions analyzed |
| Speed | Hours to review and score calls | Real-time analysis and alerts |
| Consistency | Varies by reviewer, prone to bias | Consistent scoring against defined criteria |
| Compliance Detection | Violations found days/weeks later | Real-time alerts enable immediate correction |
| Coaching Specificity | Generic feedback based on small sample | Specific examples from actual conversations |
| Scalability | Limited by QA team capacity | Scales infinitely without additional staff |
| Cost | High labor costs for manual review | 60-80% lower QA costs |
| Trend Identification | Difficult with limited data | Pattern recognition across all interactions |
Automation matters in healthcare because consistency saves lives and prevents violations. A single missed compliance check costs exponentially more than the technology investment.
G. The future of conversation intelligence in healthcare
Explore how AI-driven conversation intelligence is evolving inside healthcare. You discover what’s coming next, from real-time compliance alerts to predictive patient risk signals.
1. Real‑time AI‑powered alerts for compliance violations
Real‑time alerts will suggest next best actions during live calls. Agents will see prompts to read missing disclosures, clarify confusing phrases, or escalate sensitive situations.
Several HIPAA‑aware AI vendors now offer healthcare‑specific assistants that run inside existing workflows. Conversation intelligence will increasingly power these assistants with context from recent interactions.
2. Predictive analytics for patient risk identification
Predictive analytics will help you spot patterns that indicate churn risk, no‑show likelihood, or rising frustration before they surface as complaints.
By combining conversation sentiment, topic patterns, and historical outcomes, models will support targeted outreach and proactive care coordination. This aligns with the broader growth of AI in healthcare across the US and Europe over the next decade.
3. Integration with clinical workflows
Conversation intelligence will integrate more deeply with ambient documentation and clinical decision support. Notes and summaries from service calls may feed into clinical records, task lists, or triage systems, always with clinician review.
The goal is not to replace clinical judgment but to remove manual documentation overhead and keep communication aligned with what happens in the clinic or at home.
Emerging trends from current deployments
Current case studies highlight trends such as:
- Proactive follow‑up based on conversation‑defined risk.
- Stronger links between contact centers, patient portals, and remote monitoring.
- Tighter governance around AI fairness, bias, and explainability.
Organizations that invest now in high‑quality QA data and conversation analytics will find it easier to adopt these advanced capabilities safely later.
H. Getting started: what healthcare leaders should know
You get started by clarifying your primary goal, picking a focused pilot scope, and shortlisting healthcare‑ready vendors that fit your stack and risk posture. This helps you move from curiosity to an actionable roadmap with realistic timelines and ROI expectations.
Key evaluation criteria for conversation intelligence platforms:
- HIPAA compliance certification with signed BAA
- Healthcare-specific features including medical terminology accuracy and clinical workflow integration
- Real-time monitoring capabilities for compliance and quality
- EHR/EMR integration options with your existing systems
- Scalability to handle your call volume without performance degradation
- Customizable quality frameworks aligned with your standards
- PII detection and redaction built into the platform
- Audit trail and reporting meeting regulatory requirements
Questions to ask vendors:
- How do you handle HIPAA compliance and BAA requirements?
- What healthcare organizations currently use your platform?
- How does your system integrate with [your specific EHR/call center platform]?
- What’s your data retention and deletion policy?
- How do you ensure AI accuracy for medical terminology?
- What’s included in your implementation and training process?
- How do you handle system updates without disrupting operations?
- What compliance frameworks do you support out-of-the-box?
Implementation timeline & ROI expectations:
Typical implementations take 8-12 weeks from contract to full deployment. Expect 2-3 weeks for technical integration, 3-4 weeks for configuration and testing, and 2-3 weeks for staff training and rollout.
ROI becomes visible within 3-6 months. Early wins include reduced QA labor costs, improved appointment conversion rates, and caught compliance violations. Longer-term benefits like reduced staff turnover and improved patient retention compound over 12-18 months.
Organizations typically see 15-30% improvement in scheduling conversion, 60-80% reduction in QA costs, and 30-45 minutes daily time savings per clinical staff member.
Learn how Enthu.AI helps healthcare organizations automate quality assurance, ensure HIPAA compliance, and transform patient conversations into actionable insights that improve both care quality and operational efficiency.
Request for a FREE demo today!
FAQs
1. What is conversational AI in healthcare?
Conversational AI uses natural language processing to enable human-like dialogue between patients and digital systems. It powers chatbots, virtual assistants, and voice tools that automate scheduling, answer questions, and provide personalized support through natural conversation.
2. What are some examples of conversational AI in healthcare?
Examples include AI chatbots for appointment scheduling, virtual health assistants for medication reminders, voice-enabled clinical documentation systems, and automated messaging for post-discharge monitoring. These tools operate 24/7, handling routine tasks so staff focus on complex care.
3. Is conversation intelligence HIPAA compliant?
Yes, when configured with end-to-end encryption, automatic PII redaction, HITRUST-certified storage, and signed Business Associate Agreements. Always verify your vendor provides these protections before processing protected health information.



 On this page
On this page